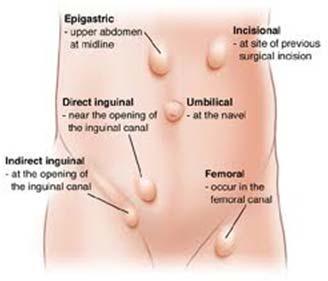
Common Forms of Hernia:
Less Common forms of Hernia:
What is a hernia?
What are the causes of Hernia?
Almost all hernias are caused by increased intra abdominal pressure due to several reasons along with weakness in the muscle. Sometimes the muscle weakness is present at birth; more often, it occurs later in life.
Commonly hernia may be caused by:
Groin Hernia:
A groin hernia occurs when the intestine bulges through the opening in the muscle in the groin area. A reducible hernia is one which can be pushed back into the opening. When intestines or abdominal tissue fills the hernia sac and cannot be pushed back, it is called irreducible or incarcerated. A hernia is strangulated if the intestine is trapped in the hernia pouch and the blood supply to the intestine is decreased. This is a surgical emergency.
There are two types of groin hernias:
An inguinal hernia appears as a bulge in the groin or scrotum. Inguinal hernias account for 75% of all hernias and are most common in men.
A femoral hernia appears as a bulge in the groin, upper thigh, or labia (skin folds surroundingthe vaginal opening). Femoral hernias are ten times more common in women.They are always repaired because of a high risk of strangulation.
Inguinal hernia signs and symptoms include:
One should be able to gently push the hernia back into abdomen in lying down posture. If not, applying an ice pack to the area may reduce the swelling enough so that the hernia slides in easily. Lying down with higher pelvis and head down may also help in pushing the hernia back into abdomen.
Treatment options:
Open hernia repair—An incision is made near the site and the hernia is repaired with mesh or by suturing (sewing) the muscle.
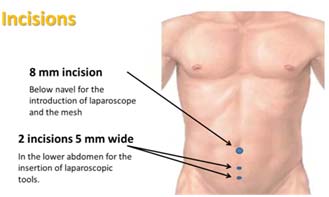
Laparoscopic hernia repair—The hernia is repaired by mesh or sutures inserted through instruments placed into small incisions in the abdomen.
Laparoscopic Hernia Surgeries:
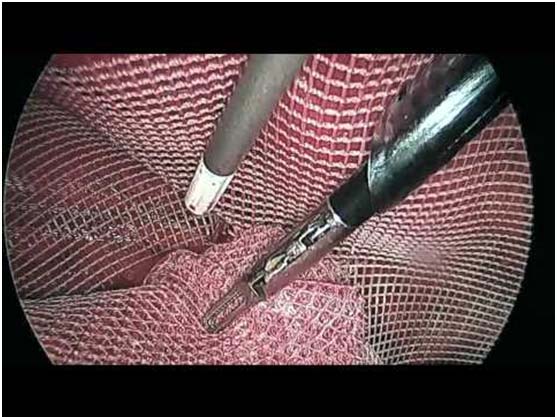
The surgeon will make several small punctures or incisions in the abdomen. Ports (hollow tubes) are inserted into the openings. The abdomen is inflated with carbon dioxide gas to make it easier to see the internal organs. Surgical tools and a laparoscopic light are placed into the ports. The hernia is repaired with mesh and sutured or stapled in place. The repair is done as a TransAbdominalPrePeritoneal (TAPP) procedure, which means the peritoneum (the sac that contains all of the abdominal organs) is entered, or the repair is done as a Totally ExtraPeritoneal (TEP) procedure. Newer techniques for laparoscopic hernia repair like eTEP (enhanced view totally extra peritoneal repair ) is being frequently offered to the patients.
Mesh
Surgical mesh is a medical device that is used to provide additional support to weakened or damaged tissue. The majority of surgical mesh devices currently available for use are constructed from synthetic materials or animal tissue.
Surgical mesh made of synthetic materials can be found in knitted mesh or non-knitted sheet forms. The synthetic materials used can be absorbable, non-absorbable or a combination of absorbable and non-absorbable materials.
Non-absorbable mesh will remain in the body indefinitely and is considered a permanent implant. It is used to provide permanent reinforcement to the repaired hernia.
For inguinal hernia repair we use non absorbable meshes preferably PVDF mesh.
How to prepare for the Surgery
*Home Medication
Patient has to bring all the medications and vitamins that he or she has been taking, so that doses may be adjusted before the surgery.
*Anesthesia
Pre - anesthetic check up is done a day before the surgery particularly to know about the allergies, neurologic disease (epilepsy, stroke), heart disease, stomach problems, lung disease (asthma, emphysema), endocrine disease (diabetes, thyroid conditions), or loose teeth and if there is any history of smoking, alcohol, or drugs, or if there is any history of nausea and vomiting with anesthesia.
*Quitting smoking before surgery can decrease rateof respiratory and wound complications and increase chances of staying smoke- free for life.
Length of Stay
Patients usually go home the same day. A few might stay overnight if there are issues such as complicated hernias or due to some medical problems which need to be taken care of.
Umbilical and Ventral Hernias:
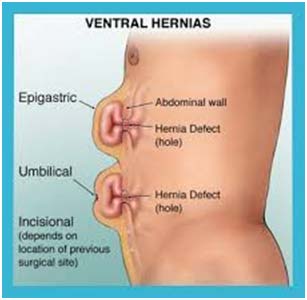
What is a ventral hernia?
A ventral hernia is a bulge of tissues through an opening of weakness within the abdominal wall muscles. It can occur at any location on the abdominal wall.
Most of the time they are called incisional hernias because they form at site of past surgical incisions where the abdominal wall is weak.
In a strangulated ventral hernia, intestinal tissue gets tightly caught within an opening in the abdominal wall. This tissue can’t be pushed back into the abdominal cavity, and its blood flow is cut off. This type of ventral hernia is an emergency requiring surgery.
What are the risk factors of developing a ventral hernia?
The risk factors include:
What are the symptoms of ventral hernia?
Diagnosis?
A physical examination is most appropriate for the diagnosis of a ventral hernia. Sometimes certain imaging investigations are required to confirm the diagnosis, which include an abdominal ultrasound or a CAT scan or an MRI.
What is the treatment?
Ventral hernias are treated surgically.
Benefits of laparoscopic removal include the following:
These are a few concerns about open surgery:
Meshes in ventral Hernia:
These includes non-absorbable and synthetic, non-absorbable and synthetic with a barrier, synthetic and partially absorbable, combined and biological materials.
1. Non-absorbable and synthetic materials
Among the various groups, prosthetic materials falling under this category especially the polypropylene (PP), polyester (PE), and expanded polytetrafluoroethylene (ePTFE) based meshes are the one used extensively.
2. Non-absorbable and synthetic with a barrier
Prosthesis with either an absorbable or a nonabsorbable barrier is used for preventing bowel adhesions when it placed intraperitoneally. This mesh is engineered in such a way that barrier on one of their faces to facilitate direct contact with the viscera. Here the barrier minimize the biological response, provide the limited opportunity for initial adhesion to the material.
3. Synthetic and partially-absorbable meshes
The purpose of constructing partially absorbable mesh is mainly to reduce the density of the biomaterial and its subsequent inflammatory reaction while maintaining the intraoperative handling characteristics and long-term wound strength.
4. Combined Meshes
The main purpose of combined mesh material is to prevent the complications by taking advantages of the best traits from 2 different meshes. In case of polyester and PTFE combined meshes, former allows the abdominal wall tissue in-growth whereas later prevent the occurrence of intestinal adhesion achieved through different pore size of the mesh. Manufactures are developing various combination mesh materials in an attempt to provide surgeons with an improved synthetic mesh.
5. Biological meshes
Even though currently available biologic meshes are seemed to have different origin, these are all common in taking collagen rich tissues from human or animals, stripping of all cellular contents and stabilizing the resultant extracellular protein structure to act as a collagen scaffold for the in growth and deposition of fibroblast and collagen respectively. Because these materials induce angiogenesis for the remodeling of the tissue, potentially resist infection, and they have a moderately good success rate for salvaging contaminated and infected fields, especially when placed with wide overlap.