When a person’s weight is higher than what is acknowledged as healthy for their height, that person is overweight or obese. Overweight and Obesity are defined as abnormal or excessive fat accumulation that may damage your health. These people live shorter lives and live with more chronic diseases.
We use body mass index (BMI) to identify overweight and obesity. BMI is defined as a person’s weight (in kilograms) divided by the square of height in meters. The higher the BMI, the higher the risk of mortality of a person. That’s because obesity is more than extra weight – it’s a complex disease that can affect the whole body. The difference between being overweight and obese is made by looking at the BMI and the relative mortality risk increase. A person whose BMI is in the range of 18.0 to 22.4 is considered at normal weight; an overweight person has a BMI of 22.5 to 27.4. Obesity is BMI 27.35 to 37.4 without medical complications. If your BMI is 32 with associated medical complications you can opt for Bariatric surgery for cure.
Obesity is a threat to health and associated with multiple medical complications, including:
- Hypertension
- Diabetes Mellitus
- Obstructive sleep apnea
- Cardiovascular disease
- Pancreatitis
- Dyslipidemia
- Non-alcoholic fatty liver disease
- Polycystic ovarian syndrome
- Infertility
- stroke
- Cataracts
- Cancer (uterus, cervix, prostate, kidney, colon, esophagus, pancreas, liver)
- Osteoarthritis
Obesity is associated with a lower life expectancy, because obese individuals are at higher risk of so many medical complications. Obesity is influenced by a vast variety of factors, including genetic, lifestyle, environmental and behavioral factors. Treatment for obesity must be multidisciplinary, as so many factors play a role in obesity. The first step is making behavioral and lifestyle changes. This can be followed by a more personalized exercise and nutrition plan.
Unfortunately, many patients who are overweight or obese have tried dieting programs and exercising for years. Despite many years of effort, some people cannot attain the desired results.
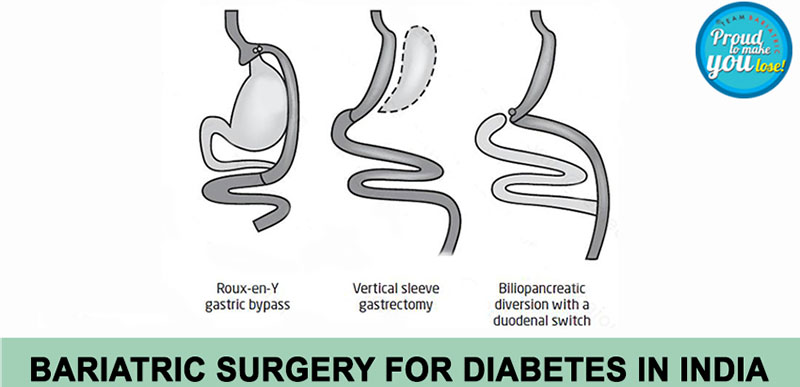
We now know that obesity is not just a disease treated by attempts, as our society wants us to believe. Obese people need extra appliance to achieve healthy weight. Bariatric surgery, together with a comprehensive lifestyle change is time and again the only way to achieve long term results.